In our news too there has been a lot of talk of testing. There have been calls to increase our testing capacity, make tests faster, test for antibodies, make different types of testing kits available in India… These discussions can seem muddled even if you know how testing is done for SARS-CoV-2, and it must seem a right mess if you don’t. So, let’s look at how these tests are done.
Viruses, including the coronaviruses, are neither dead nor alive. They have genetic material that codes for their proteins but lack the genes that allow them to make copies of themselves – they can’t reproduce without help. SARS-CoV-2 is no exception – it ‘infects’ us to make copies of itself. It finds its way into our lungs through our nose and eyes. There, it latches onto the cells lining our lungs and injects its genetic material into them. Unknowingly, our cells begin to make many copies of the viral genes. Very quickly the viral genes make lots of viral proteins, and lots copies of the virus can now be released into our respiratory tracts from our very own cells to continue the cycle of infection. As this is happening, the infected cells send out a signal to trigger our immune system, which begins to make antibodies against the viral proteins. These antibodies come in two flavours. The first are the IgM antibodies. The immune system rapidly churns these out to deal with the infection at hand. The IgMs fade away as the infection subsides. The second are the IgG antibodies. These are made at leisure, but they last in our bodies for much longer. The IgG antibodies are the ones that give us ‘immunity’, were we to encounter the same virus again in the future.

If a person were ill and showing symptoms – cough and a fever – it’s likely that they have the virus reproducing within them. But it could be SARS-CoV-2 or some other virus giving the patient the common cold. After all, other coronaviruses and influenza viruses show similar initial symptoms. So, doctors would take a swab from the back of the nose and throat of the patient and run a test to check if it’s SARS-CoV-2.
When new diseases emerge, scientists can rapidly isolate the genetic material of the causative agent – RNA or DNA as the case maybe – and read its entire genetic code. For example, the SARS-CoV-2 genome was sequenced and released into the public domain a mere few weeks after Covid-19 was first described. Once the sequence of the genome is known, it can be compared to genomes of other coronaviruses. In many parts these genomes are likely to be very similar since they belong to the same family of viruses. But in some parts, the sequences will be unique to SARS-CoV-2. These unique bits are goldmine to scientists. They can now design extremely specific detection ‘probes’ against these unique bits. And because they are designed to be so specific to SARS-CoV-2, they will be able to distinguish between SARS-CoV-2 and any other coronaviruses.

The test itself – qPCR – is commonly used in many research and diagnostic labs to measure quantities of genetic material (‘q’ for quantitative). First, all the genetic material on the swab – DNA from the patient and RNA from the virus – is extracted into a tube. Into the tube is mixed the probe and a cocktail of enzymes and other goodies. The enzymes are special. If you give them the right conditions, they use the starting genetic material as a template and, with the help of the goodies, they churn out many exact copies of it (this is the PCR, or the ‘polymerase chain reaction’). As the copies of the genetic material increase, the probe finds an increasing number of targets to attach to. The probe is designed such that when it finds and binds to its target it emits a fluorescent signal that the qPCR machine can detect. (When there’s no target, the fluorescent signal from the probe is jammed by a ‘quencher’.) So, if the patient’s swab had viral RNA the fluorescent signal would get increasingly bright – a SARS-CoV-2 ‘positive’. Importantly, when testing for SARS-CoV-2, WHO asks that two probes be used to be doubly sure that it is SARS-CoV-2.
While this is the essence of how testing is done, different qPCR kits tinker with these elements – the combinations of probes used, the cocktail of enzymes, their associated goodies – to make the test faster. Some tests even skip the probe. But they get specificity of detection by fiddling with the mix of goodies such that only if the SARS-CoV-2 genetic material is present will the PCR work. In India, only kits that have been approved by the Indian Council of Medical Research can be used at centers that have been approved by them.
qPCR is the ‘gold standard’ in diagnostics, but it requires high-end equipment and infrastructure. In many hospitals outside of urban India, facilities to support such testing are not available. For such ‘point-of-care’ diagnostics there are many solutions. One such, that has been widely used in the diagnosis of drug resistant tuberculosis, is now being adapted to test for SARS-CoV-2. It is also a qPCR system, but the entire biology and technology around it has been made portable and compact and doesn’t require extensive technical expertise to run.
But qPCR is not the only way of looking for the virus. Techniques like LAMP, SHERLOCK, and DETECTR methods can also be used for molecular diagnostics. The general principle of these assays is the same as qPCR – identify unique bits of genetic material and look for them in the swab. But the way in which these methods ‘look for the virus’ are a little different. While the PCR enzymes need the temperature to rise and fall in a cyclical way to make copies of the viral genetic material, the enzymes in LAMP can do this without changing the temperature. A second trick that the LAMP test uses is that its soup of goodies lets you make vastly more copies of the viral genetic material. These qualities not only speed up the time taken for testing, but they also mean that you don’t need special qPCR machines to run the test. There is a drawback though – it’s much harder to use two viral-probes in this test. As a result, testing facilities would have to send samples to larger testing centers to confirm with a second probe that the sample was positive. Two-probe assays are not impossible, though. In fact, the Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST) in Trivandrum has developed such an assay and it is being validated by ICMR.
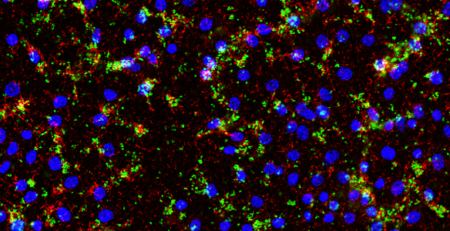
All the tests we’ve spoken of so far will be useful if a person were ill with the symptoms of Covid-19. But if someone had recovered from it, they would have cleared away the virus. The molecular diagnostics we’ve discussed so far would miss this person. While this is not consequential for treating the person – they’ve recovered, after all! – it is important to understand disease progression in a community and identify individuals who might be immune within that community. If a person had recovered from Covid-19, they likely have antibodies against the SARS-CoV-2 proteins in their blood. And depending on how long ago they were ill, they might have the IgM (early) or IgG (long-term) flavours of antibodies. This can easily be tested for. The essence of this kind of antibody testing relies on the principle that antibodies have very specific interactions with the proteins they were raised against. So, if a sample of the person’s blood were brought in contact with some synthetic viral protein, the antibodies in their blood would bind to it and this binding could be detected. The two methods that use this principle are the ELISA and the rapid antibody test. ELISA tests can be extremely specific and sensitive but the test itself needs to be done in a lab with specialized equipment.
The rapid antibody test can be done anywhere. It is often designed as a home pregnancy kit and all it needs is a drop of blood from a finger-prick that’s placed on the strip in the test. By capillary action, the fluid travels up the strip. As it does so it encounters three molecular bands that have been drawn on the strip. The first band on the strip is that of the synthetic viral protein. It’s usually been coated onto the surface of something visible such as gold nanoparticles. If the person’s blood contains antibodies it binds to these viral proteins and continues to travel up the strip taking the gold particles with it. The next two bands consist of other antibodies that will bind to any old IgM and IgG antibodies. If the person’s antiviral antibodies are of the IgM type the gold particles will get stuck at the IgM band, and if their antiviral antibodies are of the IgG type they’ll stop at the IgG band. So, just by the prick of a finger, this test can tell you whether someone has had SARS-CoV-2 infection in the recent past or a while ago.

Antibody tests are much harder to get right and are slower to develop for emerging diseases. There are many reasons for this, but probably the most important is that it’s not easy to guess which part of which viral protein the body might make antibodies against. It’s also possible that this could be different in different people, and finally, it’s possible that the antibody that’s made binds proteins from other coronaviruses and so is not specific to SARS-CoV-2. But when it’s got right, antibody tests are extremely useful.
As we approach the end of the lock-down, we need to consider our exit strategy. May 17th is no magical end to the pandemic, but we have now identified regions that need particular attention. As the country cautiously takes steps towards easing restrictions, these are the regions where test-trace-isolate will likely be aggressively implemented.