Webinar recording
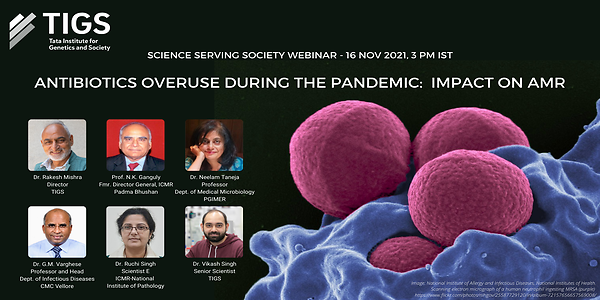
16 November 2021, 3 pm IST
Zoom webinar
Moderator:
Dr. Vikas Singh, Senior Scientist, TIGS
Opening remarks:
Dr. Rakesh Mishra, Director, TIGS
Chair:
Prof. N.K. Ganguly, Former Director General, ICMR
Presentations:
- ‘The Antimicrobial Resistance Scenario in India’ by Dr. Neelam Taneja, Professor, Department of Medical Microbiology, PGIMER
- ‘The Burden of Antibiotic Overuse during the COVID-19 Pandemic’ by Dr. G.M. Varghese, Professor and Head, Department of Infectious Diseases, CMC Vellore
- ‘Novel Strategies for Diagnosis and Treatment Due to Multi-Drug Resistant Bacteria’ by Dr. Ruchi Singh, Scientist E, ICMR-National Institute of Pathology
Panel discussion with speakers
Highlights
Dr. Rakesh Mishra in his remarks mentioned that India has done well in working towards self-sufficiency in developing strategies to handle the COVID-19 pandemic. But we must now also strengthen our efforts in dealing with our other public health concerns. Antimicrobial resistance (AMR) is a silent tsunami in the making, and the misuse of antibiotics in healthcare, livestock, and fisheries needs to be addressed.
Prof. N.K. Ganguly highlighted the various aspects of AMR that need focus in India. This is a very expansive issue that needs to be dealt with at all levels: research and development, manufacturing, healthcare, and consumer behaviour.
Dr. Neelam Taneja presented an overview of the AMR scenario in India. She mentioned that besides causing a loss of human lives, AMR could also cause a reduction in GDP by 2-3.5% and a fall in livestock production by 3-8%. She explained the various factors that drive AMR in India, of which antibiotic usage tops the list. Dr. Taneja also talked about her team’s efforts in assessing resistance to various antibiotics in healthcare settings in India and among animals.Surveillance systems set up in healthcare settings are helping a great deal, but efforts in monitoring animal health are still lagging. Antibiotic stewardship efforts that have been set up need better penetration, and improvements need to be made in improving water and sanitation access throughout the country. Our efforts to address AMR in the environment also need to be improved, especially in the case of hospital waste and effluents from chemical companies.
Dr. G.M. Varghese spoke about antibiotic misuse and challenges that we faced during the COVID-19 pandemic and the lessons we have learned from them. A meta-analysis study found that though 75% COVID-19 patients were treated with antibiotics, only 8% had bacterial co-infections. One of unintended consequences of widespread empiric treatment was the mucormycosis epidemic witnessed during the second wave of the pandemic in India. He talked about three challenges in addressing AMR, i) addressing the clinician’s fear and desire to do what’s best for an ill patient, ii) the deprioritization of AMR activities during the pandemic, and iii) the complexity of addressing AMR emergence predictors during the pandemic. He also highlighted the need to move to a culture of confirmation and treatment when treating infectious diseases.
Dr. Ruchi Singh presented some of the new approaches that are being studied to detect and tackle pathogenic bacteria. She talked about the drawbacks of current methods used in diagnosis and about new phenotypic and genotypic methods that are available. She also spoke about several nonconventional technologies and approaches in dealing with AMR, such as genome editing with the CRISPR-Cas system, the development of vaccines, phage therapy, nanoantibiotics, microbiome modification.