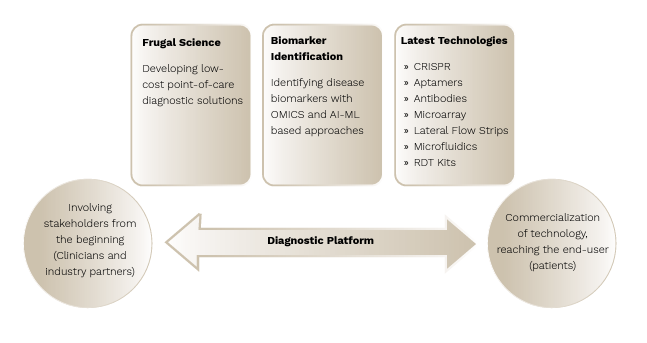
Molecular diagnostics provides powerful tools for early and more accurate diagnosis of diseases, paving the path towards personalized medicine. Accurate diagnosis is the key to the right treatment, and early diagnosis of a disease is critical for saving lives. Absence of cost-effective diagnostic methods and delayed or inaccurate diagnosis remain a health care challenge in our country. To address the existing diagnostics gap, we are developing a platform for diagnostic solutions for various infectious and rare diseases using the latest cutting-edge technologies like CRISPR.
Our diagnostics platform is focused on developing novel, low-cost, point-of-care diagnostic solutions suitable for field application in India using the latest cutting-edge technologies such as CRISPR, digital PCR, isothermal amplifications (LAMP and RPA) as well as NGS panels. The aim is to provide innovative solutions for early diagnostics that are rapid, robust, affordable, and accessible to the remotest part of the country.
- Developing Indigenous CRISPR/CAS Based Diagnostic Platform for Infectious and Rare Diseases for Field Application in India
- Molecular Diagnostics of Plant Pathogens
- Detection and Differentiation of HPV Genotypes 16, 18 and 12 other High-Risk (HR) Types for Early Screening and Patient Management
- Detection of Respiratory Pathogens (Influenza A, Influenza B, RSV A and B, SARS-CoV-2, Influenza A H1N1, Influenza A H3N2 from Clinical and Wastewater Samples
India accounts for 3% of global malaria cases and 27% of global tuberculosis cases, with a quarter of the latter being drug resistant. There are several disadvantages to the current rapid diagnostic test-based detection of malaria, and drug-resistant tuberculosis detection takes several weeks. At TIGS, we are developing CRISPR-based diagnostic solutions for malaria and tuberculosis. We have standardized the amplification of target regions for CRISPR-based detection of the malarial pathogen Plasmodium falciparum as well as Mycobacterium tuberculosis with high sensitivity and are currently in the process of performing clinical validations.
We have started work on developing CRISPR-based assay for detection of Dengue.
The platform has a keen focus on both indigenization and bolstering the stability of reagents. Our efforts have led to streamlining the production of various Cas enzymes such as Cas9, Cas12, Cas13, and Cas 14 at a lab scale. By optimizing indigenization strategies, we’ve successfully slashed reagent costs by half, and we aim to further reduce costs by indigenizing polymerases.
In rare genetic diseases, the expense and requirement for specialized infrastructure and expertise in sequencing or multiplex ligation-dependent probe amplification (MLPA) post-symptom onset pose challenges. To tackle this issue, low-cost, targeted nucleic acid-based panels stand out as an approach. Our ongoing strategy involves optimizing CRISPR-based methods for detecting SMA (Spinal Muscular Atrophy) and DMD (Duchenne Muscular Dystrophy).
Investigator: Harvinder Kour Khera
Collaborators:
Bangalore Baptist Hospital, Bengaluru
Manipal Hospital, Manipal
Jawaharlal Institute of Post Graduate Medical Education and Research (JIPMER), Puducherry
Plant diseases pose a major threat to global agriculture, potentially reducing crop yields by 17-30% annually, especially in key crops like maize and rice. Moreover, the booming seed industry of India faces challenges in meeting strict quality standards for exports. In response to this need, we planned to begin work to develop suitable detection methods utilizing advanced tools like CRISPR technology. By harnessing the power of CRISPR, we seek to provide the seed industry with innovative solutions that ensure the quality and safety of seed exports, safeguarding the interests of growers and companies alike.
Our current efforts focus on developing detection methods for various plant pathogens and the development of diagnostics of rice sheath rot caused by Sarocladium oryzae, and rice fungal blast caused by Magnoporthe.
Investigator: Harvinder Kour Khera
Collaborator:
University of Agricultural Sciences, GKVK, Bengaluru
Cervical cancer, predominantly caused by the Human Papillomavirus (HPV), poses a significant health threat to women worldwide. In India, the statistics are particularly alarming, with one woman succumbing to cervical cancer every seven minutes. It is estimated that 5% of Indian women will encounter an HPV infection at some point in their lives. However, cervical cancer stands out as the only female cancer that is not just entirely preventable but also curable when detected and treated in its early stages. Although there are multiple HPV genotypes, notably, over 80% of cervical cancers are linked to HPV genotypes 16 and 18.
Recognizing the critical nature of this issue, the World Health Organization (WHO) has advocated for a comprehensive approach to combat cervical cancer, encapsulated in the 90-70-90 model:
– 90% Vaccination: Ensuring full vaccination by the age of 15
– 70% Screening: Conducting high-performance tests by the ages of 35 and 45
– 90% Treatment: Providing timely treatment for those identified with cervical disease, whether for precancerous lesions or invasive cancer.
HPV screening plays a pivotal role in increasing the detection rate of cervical cancer, thereby significantly reducing mortality rates. While the Pap Smear assay has been commonly used, its limitations in sensitivity and scalability highlight the urgent need for DNA-based molecular diagnostics for a more accurate, robust, and scalable HPV screening program.
- Developing a qualitative PCR test for the detection and differentiation of HPV genotypes 16, 18, and the thirteen other HR types
- Development of a “do-it-yourself” self-sample collection methodology that is compatible with the assay
We have successfully developed the assay and are currently seeking industry partners for its commercialization. In terms of self-sample collection, our goal is to incorporate CDSCO approved sample collection devices into our assay’s workflow to facilitate efficient HPV detection.
Investigator: Satyaprakash Pandey
Influenza, Respiratory Syncytial Virus (RSV), and COVID-19 are three distinct respiratory viruses, each belonging to different viral families, yet collectively responsible for a significant portion of severe respiratory infections globally. These viruses often present with overlapping symptoms such as fever, cough, and difficulty breathing, complicating the clinical identification of the specific causative agent.
An innovative approach to bridge the diagnostic gap lies in environmental surveillance, particularly through the analysis of wastewater for pathogen signatures. This non-invasive method enables the monitoring of pathogen prevalence on a community-wide scale, providing a comprehensive insight into the spread and dynamics of diseases. By identifying the genetic markers of these viruses in wastewater, public health authorities can detect potential outbreaks at an early stage, allowing for prompt and targeted public health responses to curb transmission and alleviate the burden on healthcare systems.
Currently, while individual assays exist for the detection of these viruses, the development of a single multiplex assay capable of simultaneously identifying and differentiating among these pathogens stands to significantly enhance clinical diagnostics and public health management. Such an assay would enable more efficient outbreak monitoring and patient categorization, reducing the risk of cross-infection and the spread of these viruses.
Our goal is to develop a comprehensive assay capable of detecting and distinguishing among key respiratory pathogens, including Influenza A, Influenza B, RSV A and B, and Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), as well as subtyping Influenza A strains H1N1 and H3N2 from both clinical and environmental wastewater samples.
We are currently in the phase of evaluating the performance of this assay with clinical and wastewater samples and are actively seeking partnerships with industry stakeholders for its commercialization. Our efforts are directed towards cost-effective respiratory virus detection and management, ultimately contributing to more effective outbreak control and patient care.
Investigator: Satyaprakash Pandey
